In the Webinar: Women in Multiple Sclerosis, hosted by the Community of Practice of the BRAINTEASER project, we focused on the role of hormones on the onset and progression of the disease and delved deeply into several aspects of pregnancy. But first, we addressed the need for novel technological solutions to support patients, especially women, on their journey and help clinicians by providing more personalized monitoring.
Amandeep Donna about the BRAINTEASER app: “It’s what people with MS have been waiting for”

Ms. Amandeep Donna Nahal was diagnosed with multiple sclerosis when she was 17. As a member of the UK MS Society, she shared her personal experience and insights about living as a woman with MS during these 20 years. She explained how patients get all the information during a medical appointment where the clinician provides the diagnosis, which may be overwhelming sometimes. “Once you’ve left that room, you think that’s it, that was your opportunity (to ask questions) and it’s gone.” She then expresses how people with MS have been waiting for a tool like BRAINTEASER, a mobile app that provides support and follow-up. “It’s almost like there’s someone with you,” she says. The need for portable and user-centred technologies comes from the idea that patients do not talk to their neurologist every day, but every day they may be feeling different or having different symptoms. Clinically-validated solutions aim to provide another trustable source of information between clinical visits, both for patients and for physicians.
“I feel like a life touched by MS should not be lost to MS, and I hope that projects like BRAINTEASER can go towards helping that happen.”
Given the nature of Multiple Sclerosis, a long-lasting disease of the central nervous system that is addressed as an autoimmune disorder, women have a higher prevalence than men. There are some specific tools for women in the market, such as apps to follow the menstrual cycle, but they are not specific for women with MS and their particular needs. Ms. Donna reflects on how patients report during clinical visits what they remember that happened during the last months and their subjective symptoms, but for healthcare professionals to further investigate, technology can help to monitor and show exactly what has happened during that period.
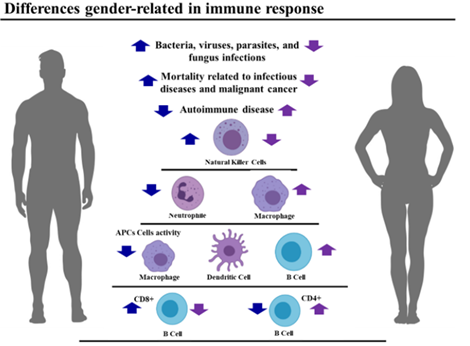
There are sex-related differences in immune response, and the shifting in MS incidence starts in puberty
Dr. Eleonora Tavazzi, from the Fondazione Istituto Neurologico Nazionale Casimiro Mondino -Pavia (Italy), presented her work about the influence of hormones in different stages of women’s life and how it affects Multiple Sclerosis. There are sex-related differences based on clinical and epidemiological observations. In pre-pubertal phases, girls and boys are affected in a similar 1 to 1 ratio, but in puberty, the statistics shift towards more incidence in women with a ratio of 3 to 1. Sex differences influence the risk of getting the disease but also how it evolves. In general, women are more prone to develop a more inflammatory disease with more relapses, whereas men have a higher risk of developing a more progressive disease course. “These clinical observations are supported by the different composition of the immune system between women and men” states Dr. Tavazzi. As men and women have different immune system compositions, men are at greater risk of infections of any nature (either viral or bacterial) and at higher risk of developing more severe complications. This is because women have an immune system richer in macrophages, B lymphocytes, and CD4+ T lymphocytes. In contrast, women are more susceptible to autoimmune diseases and inflammatory responses.
“Sex hormones as oestrogen and progesterone are not only in the structures responsible for the menstrual cycle, they are widespread throughout the central nervous system.”
For women, the clinical status and the Magnetic Functional Imaging activity related to the disease, fluctuate during the whole woman’s lifespan. One of the reasons is the fluctuation of hormones. The levels of estrogens and progesterone increase during pregnancy and then rapidly decrease after delivery, possibly mediating an immune-stabilizing process. These hormones are present also in the central nervous system, the frontal cortex, and the sensory-motor cortex of our brains, as these are responsible for the sexual behaviour that leads to reproduction. An early puberty is associated with a higher risk of developing MS and, conversely, each year of delayed menarche is associated with a 10% lesser risk of developing MS. There are several possible explanations for this phenomenon that have been widely observed in the scientific literature, including the changes in hormonal patterns or the increase of adiposity in the tissue and its relation to inflammatory molecules.
MS can affect the menstrual cycle, and the menstrual cycle can affect MS-related symptoms
“Women that were completely irregular with the menstrual cycle before the onset of the disease declared, in a significant proportion, that their menstrual irregularities appeared after the onset of the disease” states Dr. Tavazzi, highlighting the relation between hormones, the menstrual cycle, and MS. Sex hormones can modulate the release of anti-inflammatory cytokines, important proteins for cell signaling, depending on the phase of the menstrual cycle. In particular, in the first half of the menstrual cycle, there is an increase in perimenstrual symptoms and a transient worsening of MS-related symptoms. Some studies have observed an increase in relapses for 42% of the women with MS during this period. On the contrary, the use of oral contraceptives seems to be associated with a 40% lower risk of developing MS and less contrast-enhancing lesions. Notice that lesions found in the brain through magnetic resonance imaging are a biomarker of the disease. Recent studies have compared different contraceptives, being continuous oral contraceptives associated with less inflammatory activity than cyclic oral contraceptives. The widespread knowledge that mood disorders are related to the menstrual cycle phases is backed by solid scientific literature. As MS can cause damage to the brain’s white matter, it can affect brain structures such as the hypothalamus and the pituitary gland, which are responsible for the regulation of the menstrual cycle.
Women with MS report a lack of communication between patients and healthcare professionals about sexuality issues. “Sexual dysfunctions are definitely common and have a relevant impact on quality of life, but are frequently under-investigated.”
Although there is evidence that sexual function can be impaired in MS, it is a topic that has been under-investigated. Most of the studies published on this topic report that sexual dysfunctions are very frequent, up to 80% of women with MS usually declare some level of reduced sexual desire or an unsatisfying sexual life. Patients also complain about the lack of communication with their health professionals on the topic. These issues can be related to common MS symptoms that are fatigue, sensory disturbances, and mood disorders. Healthcare professionals can aid women in understanding the possible reasons for their sexuality issues when dealing with MS and provide them with additional resources and information toward a better quality of life.
“There is no proven effect of menopause on the evolution of the disease.”
When talking about menopause, we find overlapping symptoms: affective disorders, urinary and sexual dysfunction, and cognitive impairment. However, there is no proven effect of menopause on disease evolution and, therefore, no contraindications for menopause-related hormonal therapies. More research is needed to truly assess the potential role of menopause on MS.
MS is the first degenerative disease affecting women of childbearing age
Dr. Carlos de Miguel, a physician at the Hospital Gregorio Marañón in Madrid shared his knowledge about pregnancy and answered frequently asked questions from women with MS. MS is the first degenerative disease affecting women of childbearing age, and 20% of women with MS have their first pregnancy after debuting the disease. We know that the child is an organism that is genetically different from the mother, as 50% of the DNA comes from the father and, therefore, it can be considered by the woman’s body as a foreign organism. In other words, it behaves like an allogeneic transplant. However, during pregnancy, there is a mechanism so the immune system of the mother does not attack or reject the child. The complex fetus-placenta interaction secretes soluble factors that produce a reduction in pro-inflammatory cytokines, that is, starts a local immunosuppressive state, an environment where the immune system is more tolerant to foreign organisms. After birth, when the immune system returns to its prior environment, up to 30% can have a relapse.
“MS is not related to a higher number of miscarriage or preterm births, but women with a high disability may require more special treatment.”
Some of the most frequently asked questions are the following: Can I get pregnant if I am diagnosed with MS? Is there more risk of miscarriage or birth defects? Can I get epidural anaesthesia? MS has not been related to a higher number of miscarriages or preterm births, and women with a higher disability due to MS can require more special treatment. These patients may depend more on assisted fertilization methods to achieve pregnancy and have a higher risk of instrumental labor (forceps) or a C-section.
The shift in healthcare towards more personalized care, the collection of digital data, and the availability of disease-modifying therapies (DMT) such as immunotherapies for MS patients, has provided novel insights. New data shows that more relapses during the first and second trimesters of pregnancy are expected because of the DMT discontinuation, and a decrease in relapses during the third trimester with an increase after birth is expected. However, disease activity during pregnancy highly depends on previous control, and long-term outcomes are not influenced by pregnancy. If the disease is controlled, physicians recommend breastfeeding, but if it is not controlled DMT should be started acutely.
Multiple Sclerosis is not hereditary.
Multiple Sclerosis is not hereditary. A predisposition to have MS is what is inherited. The risk for the general population is 0.01%, while for first-grade relatives the risk is 3%, and single twins (who share 100% of their DNA) have only a 38% of probability. Genetics is one of the risk factors but is not a determinant. Additionally, there are no differences in general in children from the general population regarding birth weight, deficits, or gestational age.
“Overall, pregnancy is not contraindicated in women with MS, but better disease control is expected.”
Treatments of MS are often of category C, meaning that they are more based on animal studies than on humans, where adverse events for the fetus are not clearly assessed. Because of this, young women on DMTs should use proper contraceptive methods and, if they wish to become pregnant in the future, they need to consult their neurologic for DMT discontinuation if necessary. For young women with an active disease, physicians will often prioritize disease control. For women over 35, physicians will mostly prioritize pregnancy safety. There are several options available that the patient needs to discuss with the neurologist and gynecologist: To completely stop the treatment, to maintain injectable treatment during pregnancy, to use natalizumab that can be maintained until the 34th week, induction treatment through Cladribine or Alemtuzumab, or the use of immune depletors such as Ocrelizumab or Ofatumumab. Each case should be considered and evaluated individually, making a priority for disease control and fetal health. In multiple cases, DMTs are maintained during pregnancy. during pregnancy.
In conclusion, our enlightening webinar on women with multiple sclerosis united 25 participants in a meaningful dialogue driven by the invaluable insights of the expert by experience Amandeep Donna Nahal and two esteemed clinicians, Dr. Eleonora Tavazzi and Dr. Carlos de Miguel. Their comprehensive presentations addressed the significant role of hormones in multiple sclerosis throughout a woman’s life and offered current perspectives on pregnancy-related concerns, addressing frequently asked questions and sharing the latest research findings. This session not only deepened our understanding but also fostered a sense of community and support among those affected by multiple sclerosis. We extend our heartfelt thanks to our speakers and attendees for their engaging participation and look forward to continuing these important conversations in our future events.
